Curriculum

The Valley Children’s Hospital Medicine Fellowship Program has a robust curriculum focused on exploring specific areas of interest through clinical electives.
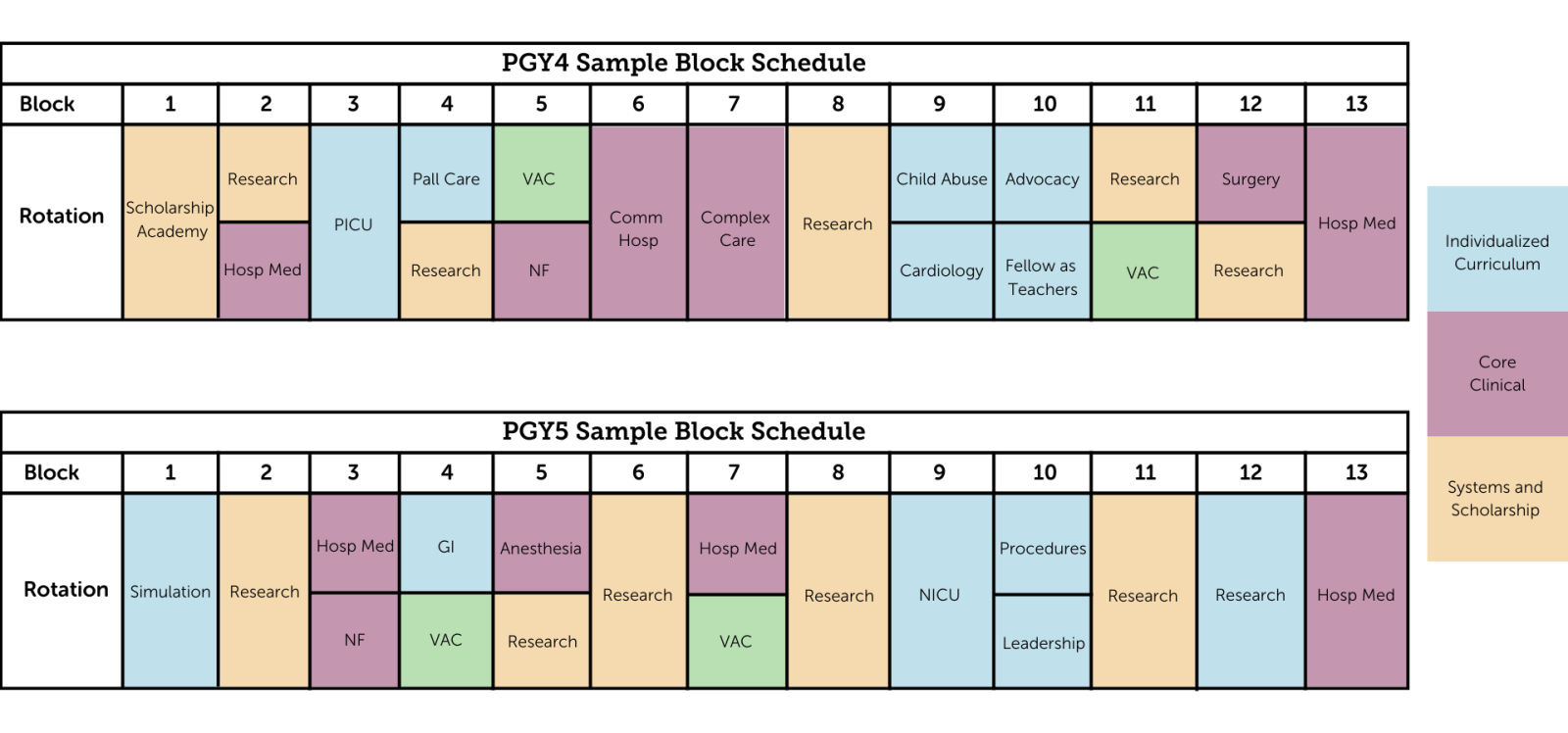
Planned Changes to Program Curriculum: Academic Year 2024-2025
| Core Clinical | Location | Year 1 | Year 2 | Total (Weeks) |
| Hospital Medicine | VCH Main Campus | 4 weeks | 2 weeks | 6 weeks |
| Resident Teaching Service | VCH Main Campus | 4 weeks | 4 weeks | 8 weeks |
| Complex Care Hospital Medicine | VCH Main Campus | 4 weeks | N/A | 4 weeks |
| Community Hospital Medicine / Newborn | Kaweah Health | 4 weeks | N/A | 4 weeks |
| Day Float | VCH Main Campus | 2 weeks | N/A | 2 weeks |
| Night Float | VCH Main Campus | 2 weeks | 2 weeks | 4 weeks |
| Anesthesia | VCH Main Campus | N/A | 2 weeks | 2 weeks |
| Surgical Co-Management | VCH Main Campus | N/A | 2 weeks | 2 weeks |
| TOTAL | 20 weeks | 12 weeks | 32 weeks |
| Individualized Curriculum | Location | Year 1 | Year 2 | Total (Weeks) |
| Clinical Selective - Critical Care (PICU/ED) | VCH Main Campus | 4 weeks | ||
| PICU | VCH Main Campus | 2 weeks | ||
| ED | VCH Main Campus | 2 weeks | ||
| Non-Clinical Selectives | ||||
| Leadership | VCH Main Campus | N/A | 2 weeks | 2 weeks |
| Fellow as Teacher | VCH Main Campus | 2 weeks | N/A | 2 weeks |
| Advocacy | VCH Main Campus | N/A | 2 weeks | 2 weeks |
| Electives | VCH Main Campus | 8 weeks | 8 weeks | 16 weeks |
| Day Float | VCH Main Campus | N/A | 2 weeks | 2 weeks |
| PHM Selective | VCH Main Campus | N/A | 4 weeks | 4 weeks |
| TOTAL | 12 weeks | 20 weeks | 32 weeks |
| Systems and Scholarship | Location | Year 1 | Year 2 | Total (Weeks) |
| Orientation / Scholarship Academy | VCH Main Campus | 2 weeks | N/A | 2 weeks |
| Research | VCH Main Campus | 14 weeks | 16 weeks | 30 weeks |
| TOTAL | 16 weeks | 16 weeks | 32 weeks |
| Vacation | 4 weeks | 4 weeks | 8 weeks |
PHM Electives
Electives include, but are not limited to:
Core Clinical Rotations
Our fellows will have ample opportunity to rotate through the full scope of our inpatient services at our 368 bed, tertiary referral center. This includes our busy teaching service, with PHM faculty, medical students and residents from both Pediatrics and Family Medicine. Fellows will serve as the leader of our interprofessional teaching teams and have graduated autonomy with clinical responsibilities and teaching. Fellows’ inpatient rounding experience will also include time on our attending-only service with a variety of our seasoned PHM faculty. They will also rotate on our admitting service, both day and night, and have primary responsibility for initial patient assessment and management, acute stabilization, resuscitation of the decompensating patient, and transfers of care. This experience also includes a primary role in patient triage and placement as our fellows will take calls from referring providers.
Fellows will rotate at our community partner site, Kaweah Health Medical Center, experiencing the full scope of community pediatric hospital medicine including the care of well newborns, opportunities for neonatal resuscitation, care of pediatric patients with straightforward conditions, and consultation on pediatric patients in the Emergency Department. Fellows will also have opportunities to work directly with and teach rotating family medicine residents. Additional time is available as part of the individualized curriculum for interested fellows.
Fellows will rotate on our dedicated complex care inpatient service, which is staffed by PHM faculty with additional expertise in the care of the medically complex hospitalized child. Fellows will gain significant experience in coordination of care, discussing end of life considerations and goals of care, leading interprofessional family care conferences, and liaising with Palliative Care and Hospice. There is also opportunity to spend dedicated time in the outpatient setting at the Charlie Mitchell Children’s Clinic, which is our medical home for children with special healthcare needs.
Fellows will spend time with our pediatric anesthesiologists in both their first and second years of training, gaining further procedural as well as sedation experience. Significant opportunity exists to customize the experience to suit fellows’ unique interests.
Fellows will rotate on pediatric surgery service and work directly with pediatric surgery attending with focus on medical management of surgical patients.
Systems and Scholarship
Fellows will have significant time dedicated to reinforcing the fundamentals of scholarship beginning early in the first year and continuing in a longitudinal fashion throughout the remainder of training. There will be significant opportunity for consultation with and mentorship by our faculty and research department.
These are woven throughout the two years, weighted to maximize time for fellows to progress and produce meaningful scholarly output. Additional time is available to suit fellows’ needs as part of the individualized curriculum.
Fellows will have longitudinal experience in quality improvement including enrollment in existing QI curriculum for trainees. There is a strong emphasis on interprofessional collaboration in quality improvement work and participation in the institutional Interprofessional Research Council will be encouraged. Based upon fellows’ individual goals and interests, additional opportunities will be provided, including serving as a facilitator for resident patient safety activities such as root cause analysis training and other experiences. Fellows will also have direct involvement organizational safety activities while on the admitting and night rotations.
Individualized Curriculum
Fellows will rotate through our PICU during their second year of training, gaining further experience in the care of the critically ill patient, stabilization, triage/patient placement, transitions of care, end of life discussions, and procedural skills. They will be precepted by Pediatric Critical Care trained physicians and have opportunities to teach resident physicians and medical students. Additional experience available for interested fellows as part of the individualized curriculum.
Fellows will rotate through our busy ED, precepted by Pediatric Emergency Medicine trained physicians, in their first year, with additional experience available as part of their individualized curriculum. Our dedicated pediatric ED sees a high volume and wide range of acuity and complexity, averaging over 100,000 visits per year. Fellows will gain experience in triage, acute stabilization and care of the critically ill patient, risk stratification for disposition, and will have significant opportunity to hone procedural skill.
Dedicated block during which fellows will receive training in areas of principles of adult learning, clinical teaching, supervision of learners, curriculum development, and feedback/evaluation.
Fellows will have dedicated block focused on developing effective leadership skills and gain exposure to a variety of physician leadership opportunities at all levels (institutional, local, regional, national).
Fellows will have a dedicated advocacy block during which they will be introduced to different types of advocacy, advocacy in medical education, and advocacy through scholarship.
Fellows have the opportunity to pursue other customizable experiences, including Business administration/Practice management, Leadership, Advocacy, Informatics, Evidence-based Medicine/pathways development, and Clinical Documentation Improvement.
Additional Electives
Fellows will have significant time dedicated to simulation experiences both initially and longitudinally, with opportunity to create a customized experience to suit their needs. Our simulation program – the first of its kind in the Central Valley to be accredited by the Society for Simulation in Healthcare – is recognized for excellence in interprofessional education and fellows will have both dedicated, fellow-only experiences as well as significant experience in real-life, interprofessional, team-based scenarios. Simulation is also utilized for introduction of new procedures as well as remediation of any areas of concern.
Fellows will work closely with our Pediatric Palliative Care team on the inpatient service, complex care service and PICU rotation, and have opportunity to spend additional time on a dedicated elective, to include home visits, engagement with hospice, and other unique experiences within the full scope of pediatric palliative care.
Fellows will achieve an understanding of pediatric infectious diseases and be able to demonstrate treatment of pediatric infectious diseases.
Fellows will achieve an understanding of various hematologic and oncologic disorders of infancy and childhood and the special diagnostic approaches to these problems.
Fellows will achieve an understanding of pediatric rheumatologic diseases such juvenile idiopathic arthritis, systemic lupus erythematosus, juvenile dermatomyositis, localized scleroderma, systemic scleroderma and pediatric vasculitis.
Fellows will achieve an understanding of both pre and post-op management of a wide range of conditions managed by pediatric surgeons from birth to young adulthood. Fellows will work with closely with a multidisciplinary team including pediatric anesthesiologists, nurse practitioners and physician assistants, occupational and physical therapists, and a host of other specialists to support each child for the best surgical outcome.
Fellows will achieve an understanding of pediatric cardiology with an emphasis on anatomy, physiology and pathophysiology. Learners will be exposed to common pediatric cardiology conditions such as heart murmurs, septal defects, valve abnormalities and complex congenital heart defects.
Fellows will achieve an understanding of pediatric gastroenterology, including work-up of rare and uncommon disorders, as well as experience in nutritional challenges and therapy in infants and children.
Fellows will achieve an understanding of pediatric nephrology and renal disorders found in infancy and childhood.
Fellows will achieve an understanding of the basics of pediatric endocrine disorders found in infancy and childhood.
Fellows will achieve an understanding of pediatric neurology, including evaluation and management of a wide variety of pediatric neurologic disorders. Valley Children's Hospital is a level 4 epilepsy center, and will provide fellows with the opportunity to learn comprehensive medical evaluation and treatment for patients with complex epilepsy.
Fellows will achieve an understanding of the basic concepts of medical genetics and their application to evaluation and screening individuals at risk for these diseases.
Fellows will achieve an understanding of the complex medical needs of high-risk neonatal patients. Formulating differential diagnosis and management of common neonatal conditions including: prematurity, respiratory distress, neonatal sepsis, apnea, congenital heart disease and other complex anomalies.
Fellows have the opportunity to work closely with our board certified child abuse specialists in the inpatient setting providing care to suspected victims of child maltreatment. There is also the opportunity to spend time at the outpatient Child Advocacy Clinic (CAC), which follows patients after discharge from the hospital to monitor physical recovery and address psychosocial needs.
Fellows have the opportunity to rotate with our pediatric critical care transport team in an experience customized to their unique needs. This includes transfer calls, patient transport, stabilization and triage, and significant experience liaising with referring community hospitals. Fellows will additionally have the opportunity to create a simulation-based scholarly product for use by future trainees.
Conferences and Didactics
Fellows will be expected to attend and present at PHM division and interdepartmental conferences over the course of their training, including:
- Weekly Tuesday Didactics
- Core Clinical Series
- Clinical Practice Guidelines
- Journal Club
- High Value Care
- Board Review
- MedEd
- Leadership
- Advocacy
- Quarterly M&M
- Longitudinal Scholarship Lectures
- Biostats, epidemiology, research methods, & QI
- Bimonthly Faculty Development
- Quarterly PHM Simulation Series
- Institutional Morbidity and Mortality
- Residency program Journal Club
- Case Conference
- Emergency Medical Response Team (EMRT) Morbidity and Mortality
- Medical Education Grand Rounds
- Health Equity Grand Rounds
- Schwartz Rounds
- Quality and Safety Series
- Leadership Series
- Wellness Lecture Series